Testicular Sperm Extraction (TESE) – Procedure, Success Rates and What to Expect
Evidence-based male fertility treatment with empathy and clarity at Kinderwunschzentrum Dresden
For many couples facing an unfulfilled wish to have a child, male infertility can be an unexpected and emotionally challenging diagnosis. When no sperm cells are found in the ejaculate, the situation can feel overwhelming. Testicular sperm extraction (TESE) offers a medically established option that may still make biological parenthood possible.
This comprehensive guide explains what TESE is, when it is recommended, how painful the procedure is, what success rates are realistic, which risks and side effects exist, and how Kinderwunschzentrum Dresden supports patients with expertise, transparency and respect.
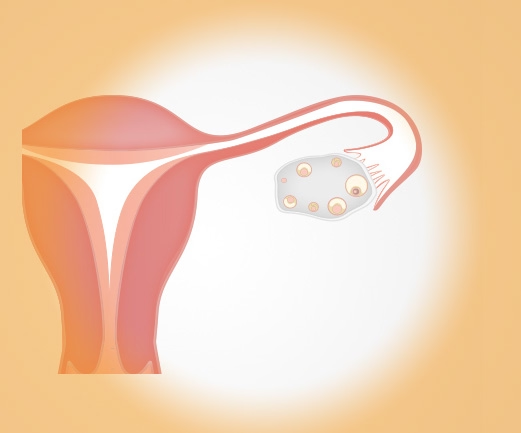
What Is Testicular Sperm Extraction (TESE)?
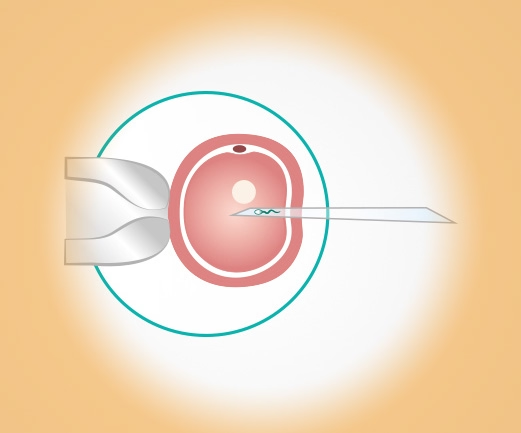
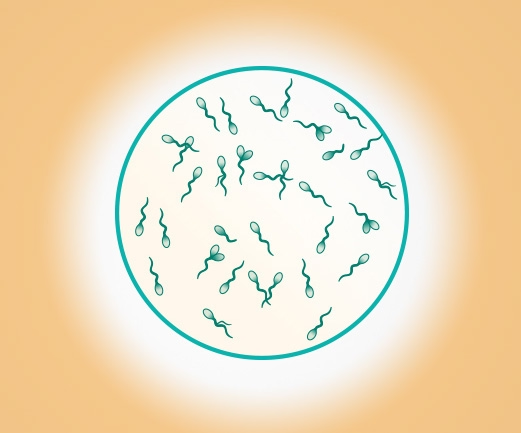
Testicular sperm extraction, commonly referred to as TESE, is a surgical procedure in which sperm cells are retrieved directly from testicular tissue. These sperm cells can then be used for assisted reproductive treatments, usually ICSI.
TESE is primarily used when sperm production is present in the testicles but sperm cells are not detectable in the ejaculate.
When Is TESE Considered?
TESE may be recommended in cases such as:
- Azoospermia (complete absence of sperm in the ejaculate)
- Blockage or damage of the sperm ducts
- Genetic or hormonal disorders affecting sperm maturation
- Unsuccessful reversal after vasectomy
Kinderwunschzentrum Dresden performs TESE according to the highest quality and safety standards and works closely with experienced urologists and andrologists to ensure optimal care. Each indication is evaluated individually before recommending the procedure.
Causes of azoospermia – why TESE may be helpful
Obstructive azoospermia
In this form, sperm are produced in sufficient numbers, but the transport pathway is blocked. Possible causes include:
- Congenital malformations of the sperm ducts
- Scarring after infections or inflammation
- Blockages caused by previous surgery
- Unsuccessful or not feasible vasectomy reversal
In cases of obstructive azoospermia, the chances of finding usable sperm are particularly good.
Non-obstructive azoospermia
Here, sperm production is reduced or partially absent. Possible causes include:
- Genetic changes (e.g. AZF deletions)
- Undescended testicles in childhood
- Severe hormonal disorders
- Previous chemotherapy or radiation therapy
- Idiopathic causes (no clear cause despite thorough diagnostics)
Even in non-obstructive azoospermia, sperm can sometimes still be found in the testicles, although the likelihood is lower and depends on individual factors.
A careful evaluation helps determine whether TESE may be a suitable option in each individual case.
How Does the TESE Procedure Work?
Pre-operative Evaluation
Before the procedure, comprehensive diagnostics are performed, including:
- Physical examination by an andrologist
- Assessment of relevant hormone levels (FSH, LH, testosterone)
- Genetic testing (karyotype analysis, AZF deletion, CFTR mutations)
- Ultrasound examination of the testicles
- Two semen analyses
This evaluation helps estimate the likelihood of finding sperm and ensures patient safety.
The TESE Operation
TESE is usually performed as a minor surgical procedure, often under local or short general anaesthesia.
The steps include:
- Small skin incision in the scrotum
- Removal of 1–3 small tissue samples of testicular tissue
- Immediate examination in the IVF laboratory
- Processing and search for motile sperm
- Freezing (cryopreservation) of retrieved sperm
The procedure is gentle, usually takes 20–40 minutes, and is generally well tolerated by patients.
How Painful Is a TESE?
A common concern among patients is whether TESE is painful.
During the Procedure
Thanks to local or general anaesthesia, pain during TESE is usually minimal or absent.
After the Procedure
Post-operative discomfort may include:
- Mild pain or tenderness
- Swelling or bruising of the scrotum
- A feeling of tightness or pressure
- Temporary sensitivity
These symptoms usually subside within a few days and can be managed with rest and pain medication if needed.
Recommended measures include:
- Gentle cooling
- Physical rest for 3–7 days
- Wearing supportive, close-fitting underwear
- Avoiding sports for approximately 2 weeks
Most patients describe the overall discomfort as manageable and well tolerated.
Chances of Success With TESE
Probability of Finding Sperm With TESE
The likelihood of retrieving sperm depends on the underlying diagnosis.
Based on clinical data and registry reports:
Obstructive azoospermia:
- Sperm retrieval rate:60–95%
- Very favorable conditions, as sperm production is usually intact
Non-obstructive azoospermia:
- Sperm retrieval rate:30–60%
- Success varies and depends strongly on individual factors
Genetic causes (e.g. AZF deletions):
- Success depends greatly on the specific AZF region involved:
- AZFa or AZFb deletions: sperm retrieval is very unlikely
- AZFc deletions:higher chances of success
These ranges reflect findings from international studies. The DIR Yearbook does not report TESE success rates separately, but it does confirm stable ICSI outcomes using TESE sperm, provided that sperm can be successfully retrieved.
Your medical team will discuss your individual chances with you in detail, based on your specific diagnosis and test results.
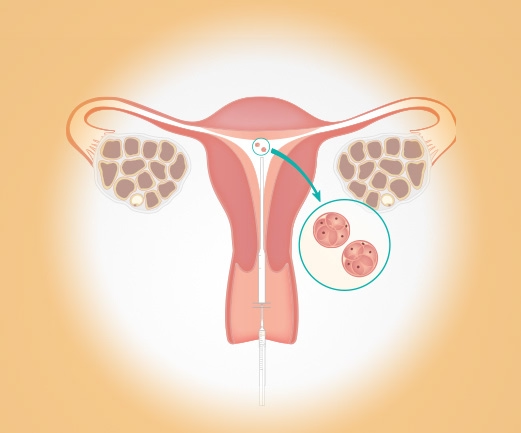
TESE Success Rates in Fertility Treatment
If sperm is successfully retrieved and used for ICSI, pregnancy rates with TESE sperm are comparable to::
- ICSI using ejaculated sperm
- ICSI after vasectomy reversal
- ICSI in cases of impaired semen parameters
Actual success rates mainly depend on:
- Quality of the TESE sperm
- Age of the female partner
- Embryo development
- Condition of the uterine lining
- Underlying causes of infertility
International data show that pregnancy rates per ICSI cycle using TESE sperm often range between 30–50%, depending largely on the woman’s age.
Advantages and Limitations of TESE
Advantages
- Enables biological fatherhood despite azoospermia
- Established, evidence-based procedure
- Often requires only a single surgical intervention
- Frozen TESE sperm can remain viable for many years when stored under optimal conditions.
Limitations and Disadvantages
- No guarantee of finding sperm
- Minor surgical risks
- Emotional stress related to uncertainty
- Not suitable for all forms of male infertility
An open discussion of benefits and limitations supports informed decision-making.
Risks and Side Effects of TESE
TESE is considered safe when performed by experienced specialists. Nevertheless, transparency about possible side effects is essential.
Common and usually mild side effects
- Swelling and bruising
- A feeling of pressure
- Mild wound pain
- Temporary sensitivity
Rare risks
- Infection
- More pronounced bruising
- Scar formation
- Temporary hormonal fluctuations
Serious complications are extremely rare. Kinderwunschzentrum Dresden follows strict surgical and hygiene standards to minimise risks.
Costs of Testicular Sperm Extraction
The total costs are made up of the following components:
Medical TESE procedure
- TESE surgery:500 euros
Laboratory processing & cryopreservation
- Processing of testicular tissue samples: 400–800 euros
- Freezing (cryopreservation): 300–600 euros
- Annual storage fees
Is TESE Covered by Health Insurance?
- German statutory health insurance covers TESE only in select medically justified cases
- Private health insurance often covers part of the costs
Kinderwunschzentrum Dresden discusses all costs clearly and transparently during the consultation appointment.
Emotional Aspects of TESE Treatment
Male infertility and surgical sperm retrieval can affect self-esteem and emotional well-being. Many patients experience uncertainty, fear or frustration during this process.
Kinderwunschzentrum Dresden addresses these concerns through:
- Respectful, non-judgmental communication
- Clear explanation of medical options
- Inclusion of both partners in counselling
- Psychological support services if desired
Emotional support is considered an integral part of medical care.
Is TESE the Right Option for You?
TESE may be appropriate in the following situations:
- Azoospermia confirmed by several semen analyses
- A hormonally normal but obstructive situation
- Non-obstructive azoospermia with residual testicular function
- Genetic considerations
- Previous vasectomy with no option for reversal
- Couples who wish to conceive using the male partner’s own sperm rather than donor sperm
The decision is always made jointly, based on medical evidence and personal circumstances.
FAQ – Common Questions About Testicular Sperm Extraction
What is the likelihood of finding sperm with TESE?
Depending on the cause of azoospermia, retrieval rates range from about 30% to over 90%. The best chances are seen in cases of obstructive azoospermia.
Is TESE painful?
The procedure itself is usually painless due to anaesthesia. Mild discomfort afterward is common but temporary.
What happens if no sperm is found during TESE?
Your medical team discusses alternative options sensitively and transparently, including donor sperm if desired.
How much does TESE cost?
The total cost is usually around 500–800 euros, including laboratory processing and cryopreservation. A detailed cost plan is provided in advance.
Is TESE sperm usually frozen?
Yes. Cryopreservation is commonly recommended to avoid repeat surgery and allow for realistic treatment planning.
Can normal success rates be achieved with TESE sperm?
Yes. When combined with ICSI, success rates can be very good under appropriate conditions.
Contact us to learn more about your individual treatment options
Testicular sperm extraction can open new possibilities when male infertility seems to limit options. With medical expertise, transparent counselling and empathetic care, Kinderwunschzentrum Dresden supports you in every step of this decision.
Schedule your confidential consultation now via Doctolib – respectful, evidence-based and individually tailored.
Dresden Fertility Center
in the Wöhrl Plaza
Prager Str. 8a
01069 Dresden
Phone +49 351 501 400-0
Fax +49 351 501 400-28
Email:
Instagram Arrange your first appointment NEW: Video consultation! Downloads Impressions
Cryobank in the Kinderwunschzentrum Dresden
Prager Str. 8a
01069 Dresden
Tel. 0351 50140019
E-Mail:
| Office hours | |
|---|---|
| Mon., Wed., Thu. | 08.00 – 19.00 Hrs |
| Tue. | 08.00 – 13.00 Hrs and 14.30 – 19.00 Hrs |
| Fri. | 08.00 – 14.00 Hrs |
Availability by telephone |
|
| Mon., Wed. | 08.00 – 13.00 Hrs and 14.30 – 18.00 Hrs |
| Tue., Thu., Fri. | 08.00 – 13.00 Hrs |
Blood sampling |
|
| Mon. - Thu. | 08.00 – 17.30 Hrs |
| Fri. | 08.00 – 13.30 Hrs |
On Tuesdays the clinic is closed from 13.00 to 14.30 Hrs! |
|
Service at the Fertility Center Dresden

To the planned child